Worried If It’s IBS… Or Something Else? Some Quick Answers
If you’re having IBS (irritable bowel syndrome) symptoms like constipation and diarrhoea, you might be wondering what’s wrong ...
Look down at your abdomen. You may not realise it, but in there you’re carrying about the surface area of a studio apartment.1 That’s your gut—and amongst its folds, twists and turns, it does such important work that it uses up 40% of your body’s total energy expenditure.2
But you already sense that—because when it’s not working properly, you feel horrible. Not only is your digestion a mess, but your mood takes a dive too. You feel fatigued, irritable and out of sync with your body.
Perhaps you’ve heard about leaky gut, but you’re not sure a) if you even believe it’s a real thing and b) if it’s relevant to you. This article gives you all the detail. Here we’ll talk about the science of leaky gut, how you can find out if you have it, and what to do about it if you do.
How do you know if you have leaky gut?
When should you be tested for leaky gut?
How do you test for gut dysbiosis?
Can leaky gut be tested on the NHS?
How to test blood for leaky gut?
What is the breath test for leaky gut?
How do you diagnose leaky gut?
How to fix leaky gut?
How long does it take to fix leaky gut?
How to heal leaky gut faster?
Where to get tested for leaky gut?
Conclusion
We all have some degree of intestinal permeability (leaky gut), but problems arise when your gut becomes too permeable. To understand this, let’s talk a bit of anatomy.
The lining of your small intestine is just one cell thick. That’s just one cell separating you from the 35 tonnes of food you’re likely to eat over your lifetime.
It may seem like a design flaw, but actually it’s part of your body’s brilliant engineering. This lining is so thin because it has to perform two opposing tasks: keeping microorganisms and toxins out of your body, while letting nutrients and essential fluids pass through.
Between the cells in your gut lining are special proteins call ‘tight junctions’. You can picture these as shoelaces. When they’re tight, the gaps between the cells close up, but when they’re loose, the gaps widen to let molecules pass through.
As mentioned, we all have some degree of leaky gut. This is because these tight junctions loosen every time we eat to allow nutrients and fluids to get into your bloodstream. Occasionally, gut microbes (and their products) get through at the same time. 3
Says immunologist Dr Jenna Macciochi, “For up to four hours after a meal, microbial endotoxins can leak into our bloodstream, triggering an immune system reaction and eliciting transient inflammation. This is known as post-prandial endotoxemia. In healthy individuals, it’s short-lived and not an issue”
But problems arise when these tight junctions stay loose for too long. This causes a consistent influx of microbes, endotoxins and large food particles, all of which stimulate the immune system. The constant inflammation can contribute to a range of chronic conditions.4
Are you wondering what causes these loose tight junctions, otherwise known as leaky gut?
Your age and genetics play a role, but so do lifestyle factors. These include:
· A Western-style diet (high in sugar and saturated fat, but low in fibre)5
· Food additives6
· Excess alcohol consumption7
· Use of non-steroidal anti-inflammatories (painkillers)8
· Stress9
· Nutrient deficiencies10
· Gut infections11
· Small intestine bacterial overgrowth12
All of these (apart from nutrient deficiencies) directly cause inflammation, and the inflammation exacerbates leaky gut. It becomes a vicious circle.
If you think any of the above apply to you, it may be worth investigating leaky gut. But the only way to be sure you have it is to test.
Certain symptoms and conditions can give you clues that it’s worth testing for leaky gut.
Leaky gut is a symptom rather than a condition. But, confusingly, it’s a symptom that can contribute to other conditions. These can be within the digestive system, including:
· Food allergies and/or sensitivities13
· Inflammatory bowel disease14
· IBS15
· Coeliac disease16
They can also be outside the digestive, such as:
· Chronic fatigue syndrome17
· Fibromyalgia18
· Depression19
· Obesity20
· PCOS21
· Rheumatoid arthritis22
· Type-1 diabetes23
Just to be clear: we don’t know whether leaky gut is driving these conditions or if it’s the other way around—but research suggests they’re connected. If you experience any of the above, it’s worth testing to see if leaky gut is related to your symptoms.
Your gut microbes play a key role in maintaining a strong gut barrier, which means gut dysbiosis is closely linked to leaky gut. But when it comes to testing, there are subtle differences.
As we discuss in Gut Health Testing – All Your Questions Answered, you have communities of bacteria, fungi, viruses, protozoa, archaea and other microorganisms living in your intestines.
Our discovery of these critters has fundamentally shifted our view of microbiology and the immune system. We used to think that some microbes were good, and some were bad. We now know that it’s more important to have a balance. When these microbes are in harmony, they support your gut function by training your immune system, synthesising vitamins and producing special fatty acids that strengthen your gut barrier.24
Dysbiosis is the opposite of this. It’s a scientific way of saying ‘gut bug imbalance’, and it can negatively affect both your gut health and your health as a whole.25 There are three types of gut dysbiosis:
These often overlap. And in any case, the net effect is the same: microbial imbalance puts stress on your body. This is because imbalanced gut microbes can induce an immune response, and the resulting inflammation can bring on leaky gut. As you learnt above, leaky gut and inflammation then fuel each other—contributing to a host of chronic conditions.
It makes sense that many of the same things that bring on leaky gut can also bring on gut dysbiosis.26 More often than not, people have both. This means the if you test positive for leaky gut, it’s reasonable to assume you have some form of dysbiosis.
But if you want to be sure you have gut dysbiosis—and you want to know whether it’s predominantly down to too few beneficial bacteria, too many potentially pathogenic bacteria or just too few bacteria altogether—your best option is to take an Ultimate Gut Health Test. This shows you exactly what microbes you have in your intestines, and how plentiful they are.
At present, the NHS doesn’t test for leaky gut. This is likely because it doesn’t recognise leaky gut as a condition.
We agree with this. Leaky gut is a symptom rather than a condition—but that doesn’t mean it’s not worth testing. This is because there is plenty of evidence to suggest that leaky gut contributes to other conditions.27 This includes the obvious ones, such as IBS, and the less obvious ones, such as diabetes. You can read more about this over at What is dysbiosis?
This means that if you’re suffering from a chronic condition (or chronic symptoms) and you suspect your gut function is involved, it’s worthwhile to test for leaky gut. You can order a test through a private lab or buy leaky gut test kit online.
The easiest way to test for leaky gut is through a urine test (more on this below), but there are a few ways you can investigate leaky gut through taking a blood sample. These include:
Serum zonulin
This is one of the proteins that regulates tight junctions in the intestines. If zonulin levels are high in the blood (serum), it suggests that your gut is more permeable than it should be.
There are a couple of issues with this test. Firstly, zonulin levels naturally fluctuate, so one reading may not be reliable.28 Secondly, the specificity of the testing method is variable, which means you can get false positives.
Zonulin antibodies
When zonulin is released into your blood, your immune system responds by making antibodies. Measuring these antibodies can therefore indicate the level of zonulin. This test is considered to be more accurate than serum zonulin, but it’s also more expensive.
Other antibody markers
If your gut is leaky, other substances such as LPS (fragments of bacterial cell wall), occludin and actomyosin (other tight junction proteins) can find their way into the bloodstream.29 Again, your immune system produces antibodies, which can then be detected in a blood sample. Like zonulin antibodies, this is a pricey way to test for leaky gut.
At present, there’s no way to test for leaky gut through a breath sample.
You can take a hydrogen and methane breath test to investigate small intestine bacterial overgrowth (SIBO). But—although SIBO can contribute to leaky gut—a positive SIBO breath test is not enough to confirm leaky gut. You can learn more about SIBO by reading SIBO Test – All Your Questions Answered.
As well as a blood test, you can test for leaky gut through looking at zonulin in a stool sample (which is included in our Ultimate Gut Health Test). You can also take a urine test for leaky gut.
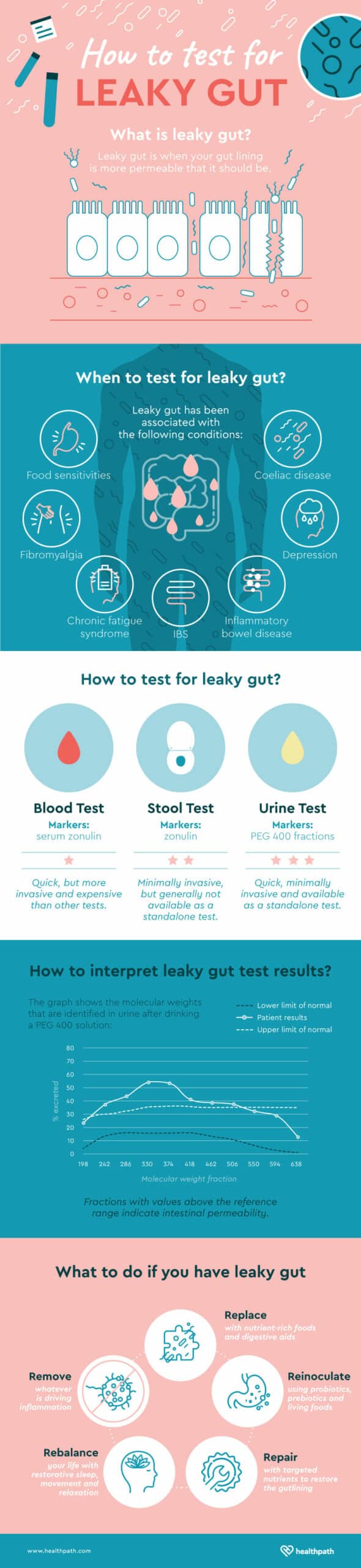
The only way to be certain you have leaky gut is to test it—and the simplest, most convenient way to do this is through performing a urine test at home.
For this test, you drink a solution called PEG 400. This solution doesn’t interfere with your body’s chemistry and it isn’t harmful. It contains substances with 11 different molecular weights.
You collect all your urine for six hours after drinking the solution, and then send it off to the lab to be analysed. By calculating how much of each substance ends up in your urine, we can work out to what degree your gut is leaky. The larger the molecular weights that get through, the leakier the gut.30
This is presented as a graph, so you can tell at a glance if your gut is more permeable than the normal range for any given molecular weight.
Remember: leaky gut is a symptom, not a condition. To restore a strong gut barrier, you’ve got to fix whatever is aggravating the symptom. This typically involves five overlapping steps: remove, replace, reinoculate, repair and rebalance.
Let’s look at each in more detail:
Remove whatever is driving inflammation. This could be a high-fat diet, a food sensitivity or even a gut infection. You may know that your diet needs some work, or you may need to work with a practitioner to explore potential pathogens.
Replace with nutrient-dense foods, plus whatever’s needed to encourage healthy digestion. Some people may just need to eat the best foods for leaky gut, while others will also require the help of digestive enzymes, digestive bitters or betaine HCl.
Reinoculate by giving your beneficial bacteria a helping hand. This can involve eating fermented foods and taking probiotic and prebiotic supplements.
Repair by taking targeted nutrients to restore the gut lining. These can include zinc, vitamin A, vitamin D, omega-3 fats and glutamine. You don’t need to take all of these—a practitioner can help you work out which is best for you.
Rebalance your life by prioritising other factors that improve leaky gut. These include good sleep, stress management and appropriate exercise.
The time needed to fix a leaky gut varies from person to person, simply because it depends on what’s causing it.
If a person has a longstanding gut infection, multiple food sensitivities and a high-stress lifestyle, it’s going to take longer to repair their gut than someone who, say, is primarily reacting to a specific food additive.
The good news is that your gut lining regenerates itself roughly every five days.31 That means that if you start making changes today, your gut can be improving physiologically within a week.
Signs of a restored gut barrier include reduced digestive symptoms, reduced food sensitivities and a lessening of other niggling symptoms. Most people can expect to notice a difference within a few months, and perhaps even a few weeks.
We’d all like to change one habit or take one supplement to fix a leaky gut, but your body doesn’t work like that. Leaky gut requires a multi-pronged approach.
In our clinical experience, people who enjoy quick improvement not only commit to eating well, but they also pay attention to the following areas:
Stress reduction. Too much stress is a huge driver of leaky gut.32 You can’t change the circumstances of your life overnight, but you can change how you react to them. To help your gut, make relaxation a non-negotiable part of your day.
Good sleep. Animal studies suggest that the body repairs and regenerates itself overnight—and that includes the gut.33 High-quality sleep one of the most important tools for repairing leaky gut.
Sensible exercise. Too little exercise isn’t good for your health, but too much exercise can worsen leaky gut.34 If you’re a gym aficionado, you may wish to rethink your routine as you give your gut time to heal.
Appropriate fasting. Animal studies also show that intermittent fasting can help to kick-start healing and rebalance the gut microbiome.35 But fasting isn’t right for everyone, and it’s best to seek professional advice first.
Clever supplementation. A therapeutic dose of the right nutrients can make a huge difference. The key is knowing what to take, and when.
To address your leaky gut as quickly as possible, you can work through these steps on your own, or you can receive targeted advice from a Functional Medicine Practitioner or Registered Nutritional Therapist.
You can visit a private lab, or you can take a leaky gut test at home. At-home testing is the most convenient option in the UK.
Here’s how the process works at Healthpath:
Intestinal permeability (more commonly known as leaky gut) is a normal physiological function—but problems arise when your gut is too leaky for too long. This can contribute to a range of symptoms both inside and outside the digestive system.
Conditions such as SIBO and dysbiosis are closely connected to leaky gut, but the only way to be certain you have leaky gut is to test for it. Leaky gut is not yet accepted as a condition by conventional medicine, but there is a large body of evidence suggesting that it’s a symptom that can drive other conditions.
If you do find out you have leaky gut, you’ll benefit from a multi-pronged approach to improving your gut health. This includes tweaking your diet, balancing your lifestyle and taking targeted supplements. The good news there’s lots you can do to take back control, and most people notice an improvement in their symptoms within a few weeks.
Author
Fiona Lawson BA (Hons) DipCNM mBANT is a Registered Nutritional Therapist and health writer. She is a member of the Complementary and Natural Healthcare Council (CNHC) and the Institute for Functional Medicine (IFM). As Content Director of Healthpath, Fiona is on a mission to help people take charge of their own health. Read more about Fiona on her practitioner page.
1 https://www.ncbi.nlm.nih.gov/pubmed/24694282
2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4253991/
3 https://onlinelibrary.wiley.com/doi/pdf/10.1002/mnfr.201300104
4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4253991/
5 https://www.ncbi.nlm.nih.gov/pubmed/28571979
6 https://www.ncbi.nlm.nih.gov/pubmed/25676324
7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4693248/
8 https://www.ncbi.nlm.nih.gov/pubmed/19255843
9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4432792/
10 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4253991/
11 https://www.ncbi.nlm.nih.gov/pubmed/12360480
12 https://www.ncbi.nlm.nih.gov/pubmed/9200287
13 https://www.ncbi.nlm.nih.gov/pubmed/16880015/
14 https://www.ncbi.nlm.nih.gov/pubmed/22731729
15 https://www.ncbi.nlm.nih.gov/pubmed/17593135/
16 https://www.ncbi.nlm.nih.gov/pubmed/10801176
17 https://www.ncbi.nlm.nih.gov/pubmed/19112401
18 https://www.ncbi.nlm.nih.gov/pubmed/18540025
19 https://www.ncbi.nlm.nih.gov/pubmed/18283240
20 https://www.ncbi.nlm.nih.gov/pubmed/28003208
21 https://www.ncbi.nlm.nih.gov/pubmed/25336505
22 https://www.ncbi.nlm.nih.gov/pubmed/1906939/
23 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4638168/
24 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4253991/
25 https://ep.bmj.com/content/102/5/257
26 http://www.altmedrev.com/archive/publications/9/2/180.pdf
27 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4290017/
28 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5569281/
29 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4253991/
30 https://www.ncbi.nlm.nih.gov/pubmed/23341423
31 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4253991/
32 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4604320/#s5title
33 https://www.nature.com/articles/srep35405
34 https://onlinelibrary.wiley.com/doi/full/10.1111/apt.14157
35 https://academic.oup.com/femsec/article/90/3/883/542224